When Lipoprotein Tests Can Be Helpful, Part I: Apo B
In my first blog, I expressed skepticism about using additional blood tests for cardiovascular disease (CVD) risk prediction beyond traditional risk factors. But I tell my trainees to “Be skeptical, not cynical,” because cynicism is the enemy of growth and improvement. Accordingly, I want to pivot to two biomarker tests that can add value in selected patients: apolipoprotein B-100 (apoB) and lipoprotein(a). This post will cover apoB.
A Primer: What Are Lipids and Lipoproteins?
This is complicated but essential and many physicians (including cardiologists) get this wrong, leading to confusion about lipid-related risk. The word “lipid” refers to two things: (i) cholesterol, a structural molecule and precursor of hormones, vitamin D, and bile acids, and (ii) triglycerides, which are fatty acids stored or burned for energy. Because cholesterol and triglycerides are oily and blood is mostly water, the body packages them into lipoproteins so the oil and water do not separate, like salad dressing in your refrigerator.
Lipoproteins are spherical particles with fats and cholesterol packaged inside and “apolipoproteins” on their surface. Apolipoproteins are the key: they make lipoprotein particles soluble and regulate their behavior and clearance. We have a wide range of lipoproteins (chylomicrons, VLDL, IDL, LDL, HDL, etc.) - you don’t need to memorize them - but one principle matters: cholesterol itself is neither “good” nor “bad”; the risk depends on which lipoprotein is carrying it.
In practice, we estimate lipoproteins indirectly by measuring the cholesterol they carry, because until recently we could quantify cholesterol more easily than the particles themselves. That is why we measure total cholesterol and calculate low-density lipoprotein cholesterol (LDL-cholesterol, what we used to call “bad” cholesterol) as the main marker of risk.
So What? Why Does This Matter to Me?
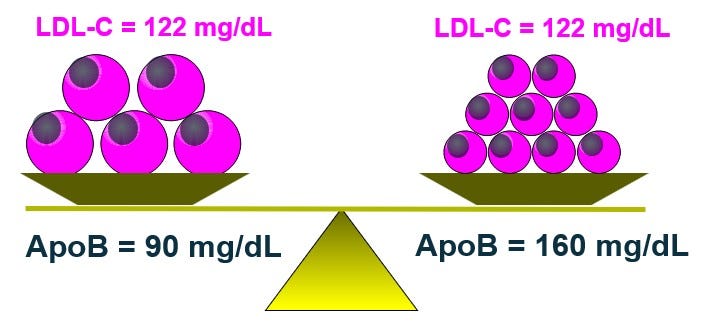
This matters clinically because your LDL-cholesterol can look fine while apoB reveals genuinely high risk. It’s tricky: when your doctor says “your LDL is good,” they actually mean “your LDL-cholesterol is in range.” That distinction is not just semantic – it is fundamental – they may say “LDL” – the lipoprotein – but they mean the cholesterol it carries and they are not the same, because the cholesterol content per LDL particle varies from person to person and even within the same person based on diet and metabolic state. Two people can have the same LDL-cholesterol but very different numbers of LDL particles depending on whether their particles are large and cholesterol-rich or small and cholesterol-poor (see figure). For a fixed LDL-cholesterol (“LDL-C” in the figure), people with small LDL particles can have 25–30% more particles. More particles – not their size – is the problem.
The pathophysiology is beyond our scope, but the core message is that arterial injury is caused by the number of LDL particles, not the amount of cholesterol inside them. Think of a traffic jam: it depends on how many cars are on the road, not how many people are in each car. Yes, they are correlated, but they are not the same. Size modulates risk, but number drives it. This is why LDL-C can look “good” while LDL particle burden and risk actually are high. Since each LDL particle contains one apoB on its surface, the apoB concentration essentially is the LDL particle concentration.
Patient Example: When LDL-Cholesterol and LDL Particle Risk Do Not Match
A 65-year-old woman is 5’3” and weighs 158 pounds. Her blood pressure is mildly elevated at 136/84 mmHg and her blood sugar is above normal. Her total cholesterol is 221, triglycerides 252, and HDL-cholesterol 48 mg/dL – all mildly abnormal. Her LDL-cholesterol is 122 mg/dL which is around the 50–60th percentile in the US, “average” to mildly elevated, and not a level most clinicians would treat. But her apoB-100 level was 160 mg/dL which is very high, at the 99th percentile (see figure, again). The discordance was predictable: elevated triglycerides, elevated blood sugar, and central adiposity metabolically lead to small, cholesterol-poor LDL particles. ApoB unmasked a high particle burden that LDL-cholesterol concealed, and it changed management. These sometimes are called “stealth” LDL.
How to Use ApoB in Clinical Care
Measuring apoB is useful when LDL-cholesterol is normal or modestly elevated but clinical context suggests concealed risk, as in people with high triglycerides, central adiposity, elevated fasting glucose, or type 2 diabetes mellitus. In such patients, “stealth” LDL and other atherogenic particles may be present without obvious signals on a standard lipid panel. To give a sense of equivalence:
If the LDL-cholesterol goal is <100 mg/dL (moderate risk), the apoB goal is <90 mg/dL.
If the LDL-cholesterol goal is <70 mg/dL (high risk), the apoB goal is <80 mg/dL.
If the LDL-cholesterol goal is <55 mg/dL (very high risk), the apoB goal is <60 mg/dL.
These thresholds align treatment with the biology that causes harm - cumulative particle exposure - rather than with cholesterol mass alone. NB: a quick, back-of-the-envelope way to approximate particle burden is to calculate “non-HDL cholesterol” by subtracting HDL-cholesterol from total cholesterol. This is an improvement over looking at LDL-cholesterol alone, but it only is an estimate because it assumes fixed relationships between lipids and lipoproteins.
When ApoB Prevents Overtreatment
ApoB also can be useful in the opposite direction. Lean women with moderately high HDL-cholesterol (often 70–90 mg/dL) and otherwise favorable metabolic markers often have LDL-cholesterol values that overestimate risk. They typically carry large LDL particles, not excess small ones, so LDL-cholesterol values of 140–150 mg/dL may not reflect elevated particle burden. A normal apoB in that setting can prevent unnecessary therapy.
Practical Considerations
ApoB once was viewed as a specialized test, but it now is inexpensive, widely available, and often similar in cost to a standard lipid panel. It does not require fasting and is analytically precise. It reflects particle burden directly and anchors decisions most reliably when LDL-cholesterol and clinical context disagree, as in the types of patients noted above.
Summary
Atherosclerosis - plaque formation in arteries that leads to CVD - is driven by cumulative exposure to atherogenic lipoprotein particles, not the cholesterol inside them. Cholesterol is just a marker for where a lipoprotein has been. Here are the take-home points:
· CVD risk is driven by particle number, not cholesterol content
· LDL-cholesterol is an indirect surrogate and can misclassify risk
· Each LDL particle contains one apoB on its surface, so the apoB concentration essentially is the LDL particle concentration.
· ApoB predicts and tracks therapy better than LDL-cholesterol
· Use apoB when context and LDL-cholesterol don’t align
ApoB is the particle-count test that addresses what LDL-cholesterol often hides. Lipoprotein(a), which I will cover next, is about inherited risk that many people never learn they carry. It often explains why some people “do everything right” yet still develop disease.

Very helpful. Thanks
Will you bring in Apo(a) in subsequent posts? And genetic testing? Particularly Familial Hyperlipidemia and the SCARB-1 gene? Perhaps this is too personal?